FDA Drug Safety Communication: Important safety label changes to cholesterol-lowering statin drugs
|
Facts about
statins
|
|
[2-28-2012] The U.S. Food and Drug
Administration (FDA) has approved important safety label changes for the class
of cholesterol-lowering drugs known as statins. These changes were made to
provide the public with more information for the safe and effective use of
statins and are based on FDA’s comprehensive review of the statin class of drugs
(see Data Summary below). The changes include the
following:
Monitoring Liver Enzymes
Labels have been revised to remove the need for routine periodic monitoring of liver enzymes in patients taking statins. The labels now recommend that liver enzyme tests should be performed before starting statin therapy and as clinically indicated thereafter. FDA has concluded that serious liver injury with statins is rare and unpredictable in individual patients, and that routine periodic monitoring of liver enzymes does not appear to be effective in detecting or preventing serious liver injury.
Adverse Event Information
Information about the potential for generally non-serious and reversible cognitive side effects (memory loss, confusion, etc.) and reports of increased blood sugar and glycosylated hemoglobin (HbA1c) levels has been added to the statin labels. FDA continues to believe that the cardiovascular benefits of statins outweigh these small increased risks.
Drug Interactions
The lovastatin label has been extensively updated with new contraindications (situations when the drug should not be used) and dose limitations when it is taken with certain medicines that can increase the risk for muscle injury (see Lovastatin Dose Limitations below).
The lovastatin label has been extensively updated with new contraindications (situations when the drug should not be used) and dose limitations when it is taken with certain medicines that can increase the risk for muscle injury (see Lovastatin Dose Limitations below).
Healthcare professionals should refer to the drug
labels for the latest recommendations for prescribing statins (also see Additional Information for Healthcare Professionals below).
Patients should contact their healthcare professional if they have any questions
or concerns about statins.
- The statin drug labels have been revised to provide
patients with more information on the safe and effective use of statins.
Patients should be aware of the following information:
- There have been rare reports of serious liver problems in patients taking statins. Patients should notify their healthcare professional right away if they have the following symptoms: unusual fatigue or weakness; loss of appetite; upper belly pain; dark-colored urine; or yellowing of the skin or the whites of the eyes.
- Memory loss and confusion have been reported with statin use. These reported events were generally not serious and went away once the drug was no longer being taken.
- Increases in blood sugar levels have been reported with statin use.
- Certain medicines should never be taken (are contraindicated) with lovastatin (Mevacor) (see Lovastatin Dose Limitations below).
- Healthcare professionals should perform liver enzyme tests before initiating statin therapy in patients and as clinically indicated thereafter. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment, therapy should be interrupted. If an alternate etiology is not found, the statin should not be restarted.
- There have been rare post-marketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. These reported symptoms are generally not serious and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
- Increases in glycosylated hemoglobin (HbA1c) and fasting serum glucose levels have been reported with statin use.
- Healthcare professionals should follow the recommendations in the lovastatin label regarding drugs that may increase the risk of myopathy/rhabdomyolysis when used with lovastatin (see Lovastatin Dose Limitations below).
- Healthcare professionals should report adverse events involving statins to
the FDA MedWatch program using the information in the "Contact FDA" box at the
bottom of this page.
Removal of routine monitoring of liver enzymes from drug labels
FDA reviewed current monitoring guidelines, including the National Lipid Association’s Liver Expert Panel and Statin Safety Task Force recommendations.1, 2 The Liver Expert Panel stated that the available scientific evidence does not support the routine monitoring of liver biochemistries in asymptomatic patients receiving statins. The Panel made this recommendation because (1) irreversible liver damage resulting from statins is exceptionally rare and is likely idiosyncratic in nature, and (2) no data exist to show that routine periodic monitoring of liver biochemistries is effective in identifying the very rare individual who may develop significant liver injury from ongoing statin therapy. The Panel believed that routine periodic monitoring will instead identify patients with isolated increased aminotransferase levels, which could motivate physicians to alter or discontinue statin therapy, thereby placing patients at increased risk for cardiovascular events.1 The National Lipid Association’s Statin Task Force also stated that routine monitoring of liver function tests is not supported by the available evidence.2
FDA reviewed post-marketing data to evaluate the risk of clinically serious hepatotoxicity associated with statins. FDA had conducted several post-marketing reviews of statins and hepatotoxicity between years 2000 and 2009 by searching the Agency’s Adverse Event Reporting System (AERS) database. Those reviews consistently noted that reporting of statin-associated serious liver injury to the AERS database was extremely low (reporting rate of ≤2 per one million patient-years). FDA’s updated review focused on cases of severe liver injury, defined as a 4 (severe liver injury) or a 5 (death or liver transplant) using the Drug Induced Liver Injury Network (DILIN) liver injury severity scale, which were reported to AERS from marketing of each statin through 2009. Cases meeting those criteria were further assessed for causality. Seventy-five cases (27 cases with a severity score of 4, and 48 cases with a severity score of 5 (37 deaths and 11 liver transplants) were assessed for causality. Thirty of the 75 cases (14 deaths, 7 liver transplantations, and 9 severe liver injury) were assessed as possibly or probably associated with statin therapy. No cases were assessed as highly likely or definitely associated with statin therapy. FDA concluded that, despite a rising use of statins as a class since the late 1990s, there has not been a detectable increase in the annual rates of fatal or severe liver injury cases possibly or probably causally associated with statin use.
FDA also reviewed cases from the DILIN and Acute Liver Failure Study Group (ALFSG), organizations that have been submitting reports to FDA of drug-associated liver injury in their liver injury outcome studies. As of January 1, 2011, DILIN had submitted 25 reports of statin-associated liver injury to FDA, 12 of which gave hospitalization as an outcome. A 2010 article from ALFSG included 133 prospectively identified cases of idiopathic drug-induced liver injury resulting in acute liver failure.3 Of these 133 patients, 15 were taking statins, and in six of these 15 individuals a statin was identified as the only potential drug to cause drug-induced liver injury.
Based on all available data, FDA has determined that all currently marketed statins appear to be associated with a very low risk of serious liver injury and that routine periodic monitoring of serum alanine aminotransferase (ALT) does not appear to detect or prevent serious liver injury in association with statins.
Cognitive adverse events
FDA reviewed the AERS database, the published medical literature (case reports and observational studies),4-13 and randomized clinical trials to evaluate the effect of statins on cognition.14-17
The post-marketing adverse event reports generally described individuals over the age of 50 years who experienced notable, but ill-defined memory loss or impairment that was reversible upon discontinuation of statin therapy. Time to onset of the event was highly variable, ranging from one day to years after statin exposure. The cases did not appear to be associated with fixed or progressive dementia, such as Alzheimer’s disease. The review did not reveal an association between the adverse event and the specific statin, the age of the individual, the statin dose, or concomitant medication use.
Data from the observational studies and clinical trials did not suggest that cognitive changes associated with statin use are common or lead to clinically significant cognitive decline.
Increases in glycosylated hemoglobin (HbA1c) and fasting plasma glucose
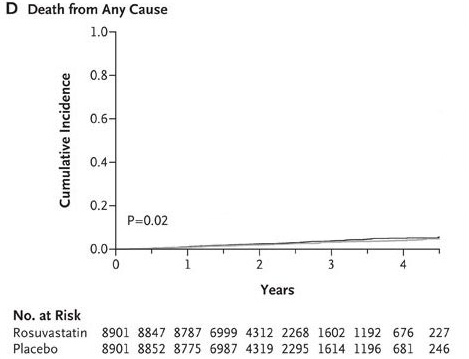
FDA’s review of the results from the Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) reported a 27% increase in investigator-reported diabetes mellitus in rosuvastatin-treated patients compared to placebo-treated patients. High-dose atorvastatin had also been associated with worsening glycemic control in the Pravastatin or Atorvastatin Evaluation and Infection Therapy – Thrombolysis In Myocardial Infarction 22 (PROVE-IT TIMI 22) substudy.18
FDA also reviewed the published medical literature.19-26 A meta-analysis by Sattar et al.,19 which included 13 statin trials with 91,140 participants, reported that statin therapy was associated with a 9% increased risk for incident diabetes (odds ratio [OR] 1.09; 95% confidence interval [CI] 1.02-1.17), with little heterogeneity (I2=11%) between trials. A meta-analysis by Rajpathak et al.,20 which included 6 statin trials with 57,593 participants, also reported a small increase in diabetes risk (relative risk [RR] 1.13; 95% CI 1.03-1.23), with no evidence of heterogeneity across trials. A recent study by Culver et al.,26 using data from the Women’s Health Initiative, reported that statin use conveys an increased risk of new-onset diabetes in postmenopausal women, and noted that the effect appears to be a medication class effect, unrelated to potency or to individual statin.
Based on clinical trial meta-analyses and epidemiological data from the published literature, information concerning an effect of statins on incident diabetes and increases in HbA1c and/or fasting plasma glucose was added to statin labels.
Lovastatin drug-drug interactions
Information regarding drug-drug interactions and contraindications and dose limitations has been added to the lovastatin label. Subsequent to the June 2011 label revisions to the simvastatin-containing products, which were based largely on the Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) trial,27 a review of drug-drug interactions with lovastatin was conducted because the physicochemical and pharmacokinetic properties of lovastatin are comparable to those of simvastatin.
Lovastatin is a sensitive in vivo cytochrome P450 3A4 (CYP3A4) substrate. Strong CYP3A4 inhibitors are predicted to significantly increase lovastatin exposure. A literature review indicates that itraconazole, a strong CYP3A4 inhibitor, increases lovastatin exposure up to 20-fold and the drug interaction appears to result in rhabdomyolysis.28 The effect of itraconazole on lovastatin exposure can therefore be extrapolated to other strong CYP3A4 inhibitors, including ketoconazole, posaconazole, erythromycin, clarithromycin, telithromycin, human immunodeficiency virus (HIV) protease inhibitors, boceprevir, telaprevir, and nefazodone.
| Previous lovastatin label | New lovastatin label |
|---|---|
Avoid lovastatin with:
|
Contraindicated with lovastatin:
|
Do not exceed 20 mg lovastatin daily with:
|
Avoid with lovastatin:
|
Do not exceed 20 mg lovastatin daily with:
| |
Do not exceed 40 mg lovastatin daily with:
|
Do not exceed 40 mg lovastatin daily with:
|
| Avoid large quantities of grapefruit juice (>1 quart daily) | Avoid large quantities of grapefruit juice (>1 quart daily) |
- Cohen DE, Anania FA, Chalasani N; for the National Lipid Association Statin Safety Task Force Liver Expert Panel. An assessment of statin safety by hepatologists. Am J Cardiol. 2006;97(8A):77C-81C.
- McKenney JM, Davidson MH, Jacobson TA, Guyton JR. Final conclusions and recommendations of the National Lipid Association Statin Safety Assessment Task Force. Am J Cardiol. 2006;97(8A):89C-94C.
- Reuben A, Koch DG, Lee WM; for the Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52(6):2065-2076.
- Orsi A, Sherman O, Woldeselassie Z. Simvastatin-associated memory loss. Pharmacotherapy. 2001;21:767-9.
- Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy. 2003;23:871-80.
- Evans MA, Golomb BA. Statin-associated adverse cognitive effects: survey results from 171 patients. Pharmacotherapy. 2009;29:800-811.
- Parker BA, Polk DM, Rabdiya V, et al. Changes in memory function and neuronal activation associated with atorvastatin therapy. Pharmacotherapy. 2010;30(6):236e-240e.
- Zamrini E, McGwin G, Roseman JM. Association between statin use and Alzheimer's disease. Neuroepidemiology. 2004;23:94-98.
- Zandi PP, Sparks DL, Khachaturian AS, et al. Do statins reduce risk of incident dementia and Alzheimer disease? The Cache County Study. Arch Gen Psychiatry. 2005;62:217-224.
- Zhou B, Teramukai S, Fukushima M. Prevention and treatment of dementia or Alzheimer's disease by statins: a meta-analysis. Dement Geriatr Cogn Disord. 2007;23:194-201.
- Beydoun MA, Beason-Held LL, Kitner-Triolo MH, et al. Statins and serum cholesterol's associations with incident dementia and mild cognitive impairment. J Epidemiol Community Health. 2011;65:949-957.
- Bettermann K, Arnold AM, Williamson J, et al. Statins, risk of dementia, and cognitive function: secondary analysis of the Ginkgo Evaluation of Memory Study. J Stroke Cerebrovasc Dis. http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2010.11.0023. Accessed January 31, 2012.
- Benito-León J, Louis ED, Vega S, Bermejo-Pareja F. Statins and cognitive functioning in the elderly: a population-based study. J Alzheimers Dis. 2010;21:95-102.
- Muldoon MF, Barger SD, Ryan CM, et al. Effects of lovastatin on cognitive function and psychological well-being. Am J Med. 2000;108:538-546.
- Muldoon MF, Ryan CM, Sereika SM, Flory JD, Manuck SB. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am J Med. 2004;117:823-829.
- Trompet S, van Vliet P, de Craen AJ, et al. Pravastatin and cognitive function in the elderly. Results of the PROSPER study. J Neurol. 2010;257:85-90.
- Feldman HH, Doody RS, Kivipelto M, et al. Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease: LEADe. Neurology. 2010;74:956-964.
- Sabatine MS, Wiviott SD, Morrow DA, McCabe CH, Cannon CP. High-dose atorvastatin associated with worse glycemic control: a PROVE-IT TIMI 22 substudy. Circulation. 2004;110(Suppl I):S834.
- Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010;375(9716):735-742.
- Rajpathak SN, Kumbhani DJ, Crandall J, Barzilai N, Alderman M, Ridker PM. Statin therapy and risk of developing type 2 diabetes: a meta-analysis. Diabetes Care. 2009;32(10):1924-1929.
- Sukhija R, Prayaga S, Marashdeh M, et al. Effect of statins on fasting plasma glucose in diabetic and nondiabetic patients. J Investig Med. 2009;57:495-499.
- Koh KK, Quon MJ, Han SH, Lee Y, Kim SJ, Shin EK. Atorvastatin causes insulin resistance and increases ambient glycemia in hypercholesterolemic patients. J Am Coll Cardiol. 2010;55:1209-1216.
- Thongtang N, Ai M, Otokozawa S, et al. Effects of maximal atorvastatin and rosuvastatin treatment on markers of glucose homeostasis and inflammation. Am J Cardiol. 2011;107:387-392.
- Kostapanos MS, Liamis GL, Milionis HJ, Elisaf MS. Do statins beneficially or adversely affect glucose homeostasis? Curr Vasc Pharmacol. 2010;8:612-631.
- Mills EJ, Wu P, Chong G, et al. Efficacy and safety of statin treatment for cardiovascular disease: a network meta-analysis of 170,255 patients from 76 randomized trials. QJM. 2011;104:109-124.
- Culver AL, Ockene IS, Balasubramanian R, et al. Statin use and risk of diabetes mellitus in postmenopausal women in the Women's Health Initiative. Arch Intern Med. 2012;172(2):144-152.
- Armitage J, Bowman L, Wallendszus K; for the Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group. , et al. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010;376:1658-1669.
- Lees RS, Lees AM. Rhabdomyolysis from the coadministration of lovastatin and the antifungal agent itraconazole. N Engl J Med. 1995;333:664-555.
Read the complete article here.