APOE-4: The Clue to Why Low Fat Diet and Statins may Cause Alzheimer's
by Stephanie Seneff
seneff@csail.mit.edu
December 15, 2009
Abstract
Alzheimer's is a devastating disease whose incidence is clearly on the rise
in America. Fortunately, a significant number of research dollars are currently
being spent to try to understand what causes Alzheimer's. ApoE-4, a particular
allele of the apolipoprotein apoE, is a known risk factor. Since apoE plays a
critical role in the transport of cholesterol and fats to the brain, it can be
hypothesized that insufficient fat and cholesterol in the brain play a critical
role in the disease process. In a remarkable recent study, it was found that
Alzheimer's patients have only 1/6 of the concentration of free fatty acids in
the cerebrospinal fluid compared to individuals without Alzheimer's. In
parallel, it is becoming very clear that cholesterol is pervasive in the brain,
and that it plays a critical role both in nerve transport in the synapse and in
maintaining the health of the myelin sheath coating nerve fibers. An extremely
high-fat (ketogenic) diet has been found to improve cognitive ability in
Alzheimer's patients. These and other observations described below lead me to
conclude that both a low-fat diet and statin drug treatment increase
susceptibility to Alzheimer's,
1. Introduction
Alzheimer's is a devastating disease that takes away the mind bit by bit over
a period of decades. It begins as odd memory gaps but then steadily erodes your
life to the point where around-the-clock care is the only option. With severe
Alzheimer's, you can easily wander off and get lost, and may not even recognize
your own daughter. Alzheimer's was a little known disease before 1960, but today
it threatens to completely derail the health system in the United States.
Currently, over 5 million people in America have Alzheimer's. On average, a
person over 65 with Alzheimer's costs three times as much for health care as one
without Alzheimer's. More alarmingly, the incidence of Alzheimer's is on the
rise. Dr. Murray Waldman has studied epidemiological data comparing Alzheimer's
with femur fractures, looking back over the last fifty years [52]. Alarmingly,
he has found that, while the incidence of femur fractures (another condition
which typically increases with age) has gone up only at a linear rate, the
increase in the incidence of Alzheimer's has gone up exponentially, between 1960
and 2010
Alzheimer's Epidemic [15]. Just between 2000 and 2006, US
Alzheimer's deaths rose by 47%, while, by comparison, deaths from heart disease,
breast cancer, prostate cancer, and stroke combined
decreased by 11%.
This increase goes far beyond people living longer: for people 85 and older, the
percentage who died from Alzheimer's rose by 30% between 2000 and 2005
[2]. Finally, it's likely these are under-estimates, as many people suffering
with Alzheimer's ultimately die of something else. You likely have a close
friend or relative who is suffering from Alzheimer's.
Something in our current lifestyle is increasing the likelihood that we will
succumb to Alzheimer's. My belief is that two major contributors are our current
obsession with low-fat diet, combined with the ever expanding use of statin
drugs. I have argued elsewhere that low-fat diet may be a major factor in the
alarming increase in
autism and
adhd in children. I have also argued that the
obesity epidemic and the associated metabolic syndrome can
be traced to excessive low-fat diet. Statins are likely contributing to an
increase in many serious health issues besides Alzheimer's, such as sepsis,
heart failure, fetal damage, and cancer, as I have argued
here. I believe the trends will only get worse in the
future, unless we substantially alter our current view of "healthy living."
The ideas developed in this essay are the result of extensive on-line
research I conducted to try to understand the process by which Alzheimer's
develops. Fortunately, a great deal of research money is currently being spent
on Alzheimer's, but a clearly articulated cause is still elusive. However, many
exciting leads are fresh off the press, and the puzzle pieces are beginning to
assemble themselves into a coherent story. Researchers are only recently
discovering that both fat and cholesterol are severly deficient in the
Alzheimer's brain. It turns out that fat and cholesterol are both vital
nutrients in the brain. The brain contains only 2% of the body's mass, but 25%
of the total cholesterol. Cholesterol is essential both in transmitting nerve
signals and in fighting off infections.
A crucial piece of the puzzle is a genetic marker that predisposes people to
Alzheimer's, termed "apoE-4." ApoE plays a central role in the transport of fats
and cholesterol. There are currently five known distinct variants of apoE
(properly termed "alleles"), with the ones labelled "2", "3" and "4" being the
most prevalent. ApoE-2 has been shown to afford some protection against
Alzheimer's; apoE-3 is the most common "default" allele, and apoE-4, present in
13-15% of the population, is the allele that is associated with increased risk
to Alzheimer's. A person with apoE-4 allele inherited from both their mother and
their father has up to a twenty-fold increased likelihood of developing
Alzheimer's disease. However, only about 5% of the people with Alzheimer's
actually have the apoE-4 allele, so clearly there is something else going on for
the rest of them. Nonetheless, understanding apoE's many roles in the body was a
key step leading to my proposed low fat/statin theory.
2. Background: Brain Biology 101
Although I have tried to write this essay in a way that is accessible to the
non-expert, it will still be helpful to first familiarize you with basic
knowledge of the structure of the brain and the roles played by different cell
types within the brain.
At the simplest level, the brain can be characterized as consisting of two
major components: the gray matter and the white matter. The gray matter
comprises the bodies of the neurons, including the cell nucleus, and the white
matter contains the myriad of "wires" that connect each neuron to every other
neuron it communicates with. The wires are known as "axons" and they can be
quite long, connecting, for example, neurons in the frontal cortex (above the
eyes) with other neurons deep in the interior of the brain concerned with memory
and movement. The axons will figure prominently in the discussions below,
because they are coated with a fatty substance called the myelin sheath, and
this insulating layer is known to be defective in Alzheimer's. Neurons pick up
signals transmitted through the axons at junctures known as synapses. Here the
message needs to be transmitted from one neuron to another one, and various
neurotransmitters such as dopamine and GABA exert excitatory or inhibitory
influences on signal strength. In adidtion to a single axon, neurons typically
have several much shorter nerve fibers called dendrites, whose job is to receive
incoming signals from diverse sources. At a given point in time, signals
received from multiple sources are integrated in the cell body and a decision is
made as to whether the accumulated signal strength is above threshold, in which
case the neuron responds by firing a sequence of electrical pulses, which are
then transmitted through the axon to a possibly distant destination.
In addition to the neurons, the brain also contains a large number of
"helper" cells called glial cells, which are concerned with the care and feeding
of neurons. Three principle types of glial cells will play a role in our later
discussion: the microglia, the astrocytes, and the oligodendrocytes. Microglia
are the equivalent of white blood cells in the rest of the body. They are
concerned with fighting off infective agents such as bacteria and viruses, and
they also monitor neuron health, making life-and-death decisions: programming a
particular neuron for apoptosis (intentional self-destruction) if it appears to
be malfunctioning beyond hope of recovery, or is infected with an organism that
is too dangerous to let flourish.
The astrocytes figure very prominently in our story below. They nestle up
against the neurons and are responsible for assuring an adequate supply of
nutrients. Studies on neuron cultures from rodent central nervous systems have
shown that neurons depend upon astrocytes for their supply of cholesterol [40].
Neurons critically need cholesterol, both in the synapse [50] and in the myelin
sheath [45], in order to successfully transmit their signals, and also as a
first line of defense against invasive microbes. Cholesterol is so important to
the brain that astrocytes are able to synthesize it from basic ingredients, a
skill not found in most cell types. They also supply the neurons with fatty
acids, and they are able to take in short chain fatty acids and combine them to
form the longer-chain types of fatty acids that are especially prominent in the
brain [7][24][36], and then deliver them to neighboring neurons and to the
cerebrospinal fluid.
The third type of glial cell is the oligodendrocyte. These cells specialize
in making sure the myelin sheath is healthy. Oligodentrocytes synthesize a
special sulfur-containing fatty acid, known as sulfatide, from other fatty acids
supplied to them by the cerebrospinal fluid [9]. Sulfatide has been shown to be
essential for the maintenance of the myelin sheath. Children born with a defect
in the ability to metabolize sulfatide suffer from progressive demyelination,
and rapid loss of motor and cognitive functions, resulting in an early death
before the age of 5 [29]. Depletion in sulfatide is a well-known
characterization of Alzheimer's, even in early stages before it has been
manifested as cognitive decline [18]. And ApoE has been shown to play a crucial
role in the maintenance of sulfatide [19]. Throughout a person's life, the
myelin sheath has to be constantly maintained and repaired. This is something
that researchers are only beginning to appreciate, but two related properties of
Alzheimer's are poor quality myelin sheath alongside a drastically reduced
concentration of fatty acids and cholesterol in the cerebrospinal fluid [38].
3. Cholesterol and Lipid Management
In addition to some knowledge about the brain, you will also need to know
something about the processes that deliver fats and cholesterol to all the
tissues of the body, with a special focus on the brain. Most cell types can use
either fats or glucose (a simple sugar derived from carbohydrates) as a fuel
source to satisfy their energy needs. However, the brain is the one huge
exception to this rule. All cells in the brain, both the neurons and the glial
cells, are unable to utilize fats for fuel. This is likely because fats are too
precious to the brain. The myelin sheath requires a constant supply of high
quality fat to insulate and protect the enclosed axons. Since the brain needs
its fats to survive long-term, it is paramount to protect them from oxidation
(by exposure to oxygen) and from attack by invasive microbes.
Fats come in all kinds of shapes and sizes. One dimension is the degree of
saturation, which concerns how many double bonds they possess, with saturated
fats possessing none, monounsaturated fats having only one, and polyunsaturated
fats having two or more. Oxygen breaks the double bond and leaves the fat
oxidized, which is problematic for the brain. Polyunsaturated fats are thus the
most vulnerable to oxygen exposure, because of multiple double bonds.
Fats are digested in the intestine and released into the blood stream in the
form of a relatively large ball with a protective protein coat, called a
chylomicron. The chylomicron can directly provide fuel to many cell types, but
it may also be sent to the liver where the contained fats are sorted out and
redistributed into much smaller particles, which also contain substantial
amounts of cholesterol. These particles are called "lipoproteins," (henceforth,
LPP's) because they contain protein in the spherical shell and lipids (fats) in
the interior. If you've had your cholesterol measured, you've probably heard of
LDL (low density LPP) and HDL (high density LPP). If you think these are two
different
kinds of cholesterol, you would be mistaken. They are just two
different kinds of containers for cholesterol and fats that serve different
roles in the body. There are actually several other LPP's, for example, VLDL
(very-low) and IDL (intermediate), as shown in the accompanying diagram.
In this
essay I will refer to these collectively as the XDL's. As if this weren't
confusing enough, there is also another unique XDL that is found only in the
cerebrospinal fluid, that supplies the nutritional needs of the brain and
nervous system. This one doesn't seem to have a name yet, but I will call it
"B-HDL," because it is like HDL in terms of its size, and "B" is for "brain
[13]"
An important point about all the XDL's is that they contain distinctly
different compositions, and each is targeted (programmed) for specific tissues.
A set of proteins called "apolipoproteins" or, equivalently, "apoproteins"
("apo's" for short) figure strongly in controlling who
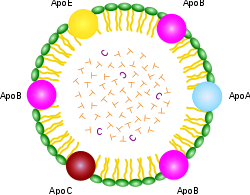
gets
what. As you can see from the schematic of the chylomicron shown at the right,
it contains a rainbow of different apo's for every conceivable application. But
the XDL's are far more specific, with HDL containing "A," LDL containing "B,"
VLDL containing "B" and "C," and IDL containing only "E." The apo's have special
binding properties that allow the lipid contents to be transported across cell
membranes so that the cell can gain access to the fats and choleseterol
contained inside.
The only apo that is of concern to us in the context of this essay is apoE.
ApoE is very important to our story because of its known link with Alzheimer's
disease. ApoE is a protein, i.e., sequence of amino acids, and its specific
composition is dictated by a corresponding DNA sequence on a protein-coding
gene. Certain alterations in the DNA code lead to defects in the ability of the
transcribed protein to perform its biological roles. ApoE-4, the allele
associated with increased risk to Alzheimer's, is presumably unable to perform
its tasks as efficiently as the other alleles. By understanding
what apoE
does, we can better infer how the consequences of doing it poorly might impact
the brain, and then observe experimentally whether the features of the
Alzheimer's brain are consistent with the roles played by apoE.
A strong clue about apoE's roles can be deduced from where it is found. As I
mentioned above, it is the only apo in both B-HDL in the cerebrospinal fluid and
IDL in the blood serum. Only selected cell types can synthesize it, the two most
significant of which for our purposes are the liver and the astrocytes in the
brain. Thus the astrocytes provide the linkage between the blood and the
cerebrospinal fluid. They can usher lipids and cholesterol across the
blood-brain barrier, via the special key which is apoE.
It turns out that, although apoE is not found in LDL, it does bind to LDL,
and this means that astrocytes can unlock the key to LDL in the same way that
they can gain access to IDL, and hence the cholesterol and fatty acid contents
of LDL are accessible to astrocytes as well, as long as apoE is functioning
properly. The astrocytes reshape and repackage the lipids and release them into
the cerebospinal fluid, both as B-HDL and simply as free fatty acids, available
for uptake by all parts of the brain and nervous system [13].
One of the critical reshaping steps is to convert the fats into types that
are more attractive to the brain. To understand this process you need to know
about another dimension of fats besides their degree of saturation, which is
their total length. Fats have a chain of linked carbon atoms as their spine, and
the total number of carbons in a particular fat characterizes it as short,
medium length, or long. The brain works best when the constituent fats are long,
and, indeed, the astrocytes are able to take in short chain fats and reorganize
them to make longer chain fats [24].
A final dimension of fats that plays a role is where the first double bond is
located in a polyunsaturated fat, which distinguishes omega-3 from omega-6 fats
(position 3; position 6). Omega-3 fats are very common in the brain. Certain
ones of the omega-3 and omega-6 fats are
essential fatty acids, in that
the human body is unable to synthesize them, and therefore depends upon their
supply from the diet. This is why it is claimed that fish "makes you smart":
because cold water fish is the best source of essential omega-3 fats.
Now I want to return to the subject of the XDL's. It is a dangerous journey
from the liver to the brain, as both oxygen and microbes are found in abundance
in the blood stream. The XDL's protective shell contains both LPP's and
unesterified cholesterol, as well as the signature apo that controls
which cells can receive the contents, as shown in the accompanying schematic.
The internal
contents are
esterified cholesterol and fatty acids, along with certain
antioxidants that are conveniently being transported to the cells packaged in
the same cargo ship. Esterification is a technique to render the fats and
cholesterol inert, which helps protect them from oxidation [51]. Having the
antioxidants (such as vitamin E and Coenzyme Q10) along for the ride is also
convenient, as they too protect against oxidation. The cholesterol contained in
the shell, however, is intentionally not esterified, which means that it is
active. One of its roles there is to guard against invasive bacteria and viruses
[55]. Cholesterol is the first line of defense against these microbes, as it
will alert the white blood cells to attack whenever it encounters dangerous
pathogens. It has also been proposed that the cholesterol in the XDL's shell
itself acts as an antioxidant [48].
HDL's are mostly depleted of the lipid and cholesterol content, and they are
tasked with returning the empty shell back to the liver. Once there, cholesterol
will be recommissioned to enter the digestive system as part of the bile, which
is produced by the gall bladder to help digest ingested fats. But the body is
very careful to conserve cholesterol, so that 90% of it will be recycled from
the gut back into the blood stream, contained in the chylomicron that began our
story about fats.
In summary, the management of the distribution of fats and cholesterol to the
cells of the body is a complex process, carefully orchestrated to assure that
they will have a safe journey to their destination. Dangers lurk in the blood
stream, mostly in the form of oxygen and invasive microbes. The body considers
cholesterol to be precious cargo, and it is very careful to conserve it, by
recycling it from the gut back to the liver, to be appropriately distributed
among the XDL's that will deliver both cholesterol and fats to the tissues that
depend upon them, most especially the brain and nervous system.
Through retrospective studies, the statin industry has been very successful
at the game of pretending that benefits derived from high cholesterol are
actually due to statins, as I have described at length in an essay on the relationship between statins and fetal damage, sepsis, cancer, and
heart failure. In the case of Alzheimer's, they are playing this game
in reverse: they are blaming cholesterol for a very serious problem that I
believe is actually
caused by statins.
The statin industry has looked long and hard for evidence that high
cholesterol might be a risk factor for Alzheimer's. They examined cholesterol
levels for men and women of all ages between 50 and 100, looking back 30 or more
years if necesssary, to see if there was ever a correlation between high
cholesterol and Alzheimer's. They found only one statistically significant
relationship: men who had had high cholesterol
in their 50's had an
increased susceptibility to Alzheimer's
much later in life [3].
The statin industry has jumped on this opportunity to imply that high
cholesterol might cause Alzheimer's, and, indeed, they have been very fortunate
in that reporters have taken the bait and are promoting the idea that, if high
cholesterol many years ago is linked to Alzheimer's, then statins might protect
from Alzheimer's. Fortunately, there exist lengthy web pages
(Cholesterol Doesn't Cause Alzheimer's) that have
documented the long list of reasons why this idea is absurd.
Men who have high cholesterol in their 50's are the poster child for statin
treatment: all of the studies that have shown a benefit for statins in terms of
reducing the number of minor heart attacks involved men in their 50's.
High cholesterol is positively correlated with longevity in people over
85 years old [54], and has been shown to be associated with better memory
function [53] and reduced dementia [35]. The converse is also true: a
correlation between
falling cholesterol levels and Alzheimer's [39]. As
will be discussed further later, people with Alzheimer's also have reduced
levels of B-HDL, as well as sharply reduced levels of fatty acids, in the
cerbrospinal fluid, i.e, impoverished supply of cholesterol and fats to the
myelin sheath [38]. As we saw earlier, fatty acid supply is essential as
building blocks for the sulfatide that is synthesized by oligodendrocytes to
keep the myelin sheath healthy [29].
The obvious study that needs to be done is to bin the men who had high
cholesterol in their 50's into three groups: those who never took statins, those
who took smaller doses for shorter times, and those who took larger doses for
longer times. Such a study would not be hard to do; in fact, I suspect something
like it has already been done. But you'll never hear about it because the statin
industry has buried the results.
In a very long term retrospective cohort study of members of the Permanente
Medical Care Program in northern California, researchers looked at cholesterol
data that were obtained between 1964 and 1973 [46]. They studied nearly ten
thousand people who had remained members of that health plan in 1994, upon the
release of computerized outpatient diagnoses of dementia (both Alzheimer's and
vascular dementia). The subjects were between 40 and 45 years old when the
cholesterol data were collected.
The researchers found a barely statistically significant result that people
who were diagnosed with Alzheimer's had higher cholesterol in their 50's than
the control group. The mean value for the Alzheimer's patients was 228.5, as
against 224.1 for the controls.
The question that everybody ought to be asking is: for the Alzheimer's group,
how did the people who later took statins stack up against the people who
didn't? In extreme understatement, the authors offhandedly remark in the middle
of a paragraph: "Information on lipid-lowering treatments, which have been
suggested to decrease dementia risk [31], was not available for this study." You
can be sure that, if there was any inkling that the statins might have helped,
these researchers would have been allowed access to those data.
The article they refer to for support, reference [19] in [46] (which is
reference [44] here) was very weak. The abstract for that article is repeated in
full here in the
Appendix.
But the concluding sentence sums it up well: "A more than a modest role for
statins in preventing AD [Alzheimer's Disease] seems unlikely." This is the best
they can come up with to defend the position that statins might protect from
Alzheimer's.
An intuitive explanation for why high cholesterol at an
early age
might be correlated with Alzheimer's risk has to do with apoE-4. People with
that allele are known to have high cholesterol early in life [39], and I believe
this is a protective strategy on the part of the body. The apoE-4 allele is
likely defective in the task of importing cholesterol into the astrocytes, and
therefore an increase in the bioavailability of cholesterol in blood serum would
help to offset this deficit. Taking a statin would be the last thing a person in
that situation would want to do.
There is a clear reason why statins would promote Alzheimer's. They cripple
the liver's ability to synthesize cholesterol, and as a consequence the level of
LDL in the blood plummets. Cholesterol plays a crucial role in the brain, both
in terms of enabling signal transport across the synapse [50] and in terms of
encouraging the growth of neurons through healthy development of the myelin
sheath [45]. Nonetheless, the statin industry proudly boasts that statins are
effective at interfering with cholesterol production in the brain
[31][47] as well as in the liver.
Yeon-Kyun Shin is an expert on the physical mechanism of cholesterol in the
synapse to promote transmission of neural messages, and one of the authors of
[50] referenced earlier. In an interview by a Science Daily reporter, Shin said:
"If you deprive cholesterol from the brain, then you directly affect the
machinery that triggers the release of neurotransmitters. Neurotransmitters
affect the data-processing and memory functions. In other words -- how smart you
are and how well you remember things."
A recent review of two large population-based double-blind placebo-controlled
studies of statin medications in individuals at risk for dementia and Alzheimer
disease showed that statins are not protective against Alzheimer's [34]. The
lead author of the study, Bernadette McGuinness, was quoted by a reporter from
Science Daily as saying, "From these trials, which
contained very large numbers and were the gold standard -- it appears that
statins given in late life to individuals at risk of vascular disease do not
prevent against dementia." A researcher at UCLA, Beatrice Golomb, when asked to
comment on the results, was even more negative, saying, "Regarding statins as
preventive medicines, there are a number of individual cases in case reports and
case series where cognition is clearly and reproducibly adversely affected by
statins." In the interview, Golomb remarked that various randomized trials have
shown that statins were either adverse or neutral towards cognition, but none
have shown a favorable response.
A common side effect of statins is memory dysfunction. Dr. Duane Graveline,
fondly known as "spacedoc" because he served as a doctor to the astronauts, has
been a strong advocate against statins on his
web page where he is
collecting evidence of statin side effects directly from statin users around the
world. He was led to this assault on statins as a consequence of his own
personal experience of transient global amnesia, a frightening episode of total
memory loss which he is convinced was caused by the statin drugs he was taking
at the time. He has now completed three books describing a diverse collection of
damning side effects of statins, the most famous of which is
Lipitor: Thief
of Memory [17].
A second way (besides their direct impact on cholesterol) in which statins
likely impact Alzheimer's is in their indirect negative effect on the supply of
fatty acids and antioxidants to the brain. It is a given that statins
drastically reduce the level of LDL in the blood serum. This is their claim to
fame. It is interesting, however, that they succeed in reducing not just the
amount of cholesterol contained in the LDL particles, but rather the actual
number of LDL particles altogether. This means that, in addition to
depleting cholesterol, they reduce the available supply to the brain of both
fatty acids and antixodiants, which are also carried in the LDL particles. As
we've seen, all three of these substances are essential to proper brain
functioning.
I conjecture that the reasons for this indirect effect are two-fold: (1)
there is inadequate cholesterol in the bile to metabolize dietary fats, and (2)
the rate-limiting effect on the production of LDL is the ability to provide
adequate cholesterol in the shell to assure survival of the contents during
transport in the blood stream; i.e., to protect the contents from oxidation and
marauding bacteria and viruses. People who take the highest 80 mg/dl dosage of
statins often end up with LDL levels as low as 40mg/dl, well below even the
lowest numbers observed naturally. I shudder to think of the probable long-term
consequences of such severe depletion in fats, cholesterol, and antioxidants.
A third way in which statins may promote Alzheimer's is by crippling the
ability for cells to synthesize coenzyme Q10. Coenzyme Q10 has the misfortune of
sharing the same metabolic pathway as cholesterol. Statins interfere with a
crucial intermediate step on the pathway to the synthesis of both cholesterol
and coenzyme Q10. Coenzyme Q10 is also known as "ubiquinone" because it seems to
show up everywhere in cell metabolism. It is found both in the mitochondria and
in the lysosomes, and its critical role in both places is as an antioxidant. The
inert esters of both cholesterol and fatty acids are hydrolyzed and activated in
the lysosomes [8], and then released into the cytoplasm. Coenzyme Q10 consumes
excess oxygen to keep it from doing oxidative damage [30], while also generating
energy in the form of ATP (adenosine triphosphate, the universal energy currency
in biology).
The final way in which statins should increase Alzheimer's risk is through
their indirect effect on vitamin D.
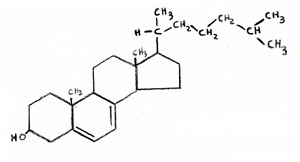
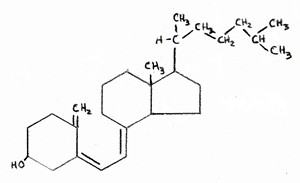
Vitamin D is synthesized from
cholesterol in the skin, upon exposure to
UV rays from the sun. In fact, the chemical formula of vitamin D is almost
indistinguishable from that of cholesterol, as shown in the two attached figures
(cholesterol on the left, vitamin D on the right). If LDL levels are
kept
artificially low, then the body will be unable to resupply adequate amounts of
cholesterol to replenish the stores in the skin once they have been depleted.
This would lead to vitamin D deficiency, which is a widespread problem in
America.
It is well known that vitamin D fights infection. To quote from [25],
"Patients with severe infections as in sepsis have a high prevalence of vitamin
D deficiency and high mortality rates." As will be elaborated on later, a large
number of infective agents have been shown to be present in abnormally high
amounts in the brains of Alzheimers patients [27][26].
Dr. Grant has recently argued [16] that there are many lines of evidence
pointing to the idea that dementia is associated with vitamin D deficiency. An
indirect argument is that vitamin D deficiency is associated with many
conditions that in turn carry increased risk for dementia, such as diabetes,
depression, osteoporosis, and cardiovascular disease. Vitamin D receptors are
widespread in the brain, and it is likely that they play a role there in
fighting off infection. Vitamin D surely plays other vital roles in the brain as
well, as powerfully suggested by this quote taken from the abstract of [32]: "We
conclude there is ample biological evidence to suggest an important role for
vitamin D in brain development and function."
6. Astrocytes, Glucose Metabolism, and Oxygen
Alzheimer's is clearly correlated with a deficiency in the supply of fat and
cholesterol to the brain. IDL, when functioning properly, is actually incredibly
efficient in cholesterol and fat throughput from the blood across cell
membranes, compared to LDL [8]. It gives up its contents much more readily than
the other apo's. And it achieves this as a direct consequence of apoE. IDL (as
well as LDL) in the blood delivers fats and cholesterol to the astrocytes in the
brain, and the astrocytes can thus use this external source instead of having to
produce these nutrients themselves. I suspect, in fact, that astrocytes only
produce a private supply when the external supply is insufficient, and they do
so reluctantly.
Why would it be disadvantageous for an astrocyte to synthesize its own fats
and cholesterol? In my opinion, the answer has to do with oxygen. An astrocyte
needs a significant energy source to synthesize fats and cholesterol, and this
energy is usually supplied by glucose from the blood stream. Furthermore, the
end-product of glucose metabolism is acetyl-Coenzyme A, the precursor to both
fatty acids and cholesterol. Glucose can be consumed very efficiently in the
mitochondria, internal structures within the cell cytoplasm, via
aerobic
processes that require oxygen. The glucose is broken down to produce
acetyl-Coenzyme A as an end-product, as well as ATP, the source of energy in all
cells.
However, oxygen is toxic to lipids (fats), because it oxidizes them and makes
them rancid. Lipids are fragile if not encased in a protective shell like IDL,
HDL, or LDL. Once they are rancid they are susceptible to infection by invasive
agents like bacteria and viruses. So an astrocyte trying to synthesize a lipid
has to be very careful to keep oxygen out, yet oxygen is needed for efficient
metabolism of glucose, which will provide both the fuel (ATP) and the raw
materials (acetyl-Coenzyme A) for fat and cholesterol synthesis.
What to do? Well, it turns out that there is an alternative, although much
less efficient, solution: to metabolize glucose
anaerobically directly in
the cytoplasm. This process does not depend on oxygen (a great advantage) but it
also yields substantially less ATP (only 6 ATP as contrasted with 30 if glucose
is metabolized aerobically in the mitochondria). The end product of this
anaerobic step is a substance called pyruvate, which could be further broken
down to yield a lot more energy, but this process is not accessible to all
cells, and it turns out that the astrocytes need help for this to happen, which
is where amyloid-beta comes in.
7. The Crucial Role of Amyloid-Beta
Amyloid-beta (also known as "abeta") is the substance that forms the famous
plaque that accumulates in the brains of Alzheimer's patients. It has been
believed by many (but not all) in the research community that amyloid-beta is
the principal
cause of Alzheimer's, and as a consequence, researchers are
actively seeking drugs that might destroy it. However, amyloid-beta has the
unique capability of stimulating the production of an enzyme, lactate
dehydrogenase, which promotes the breakdown of
pyruvate (the product of
anaerobic glucose metabolism) into
lactate, through an anaerobic
fermentation process, with the further production of a substantial amount
of ATP.
The lactate, in turn, can be utilized itself as an energy source by some
cells, and it has been established that neurons are on the short list of cell
types that can metabolize lactate. So I conjecture that the lactate is
transported from the astrocyte to a neighboring neuron to enhance its energy
supply, thus reducing its dependence on glucose. It is also known that apoE can
signal the production of amyloid-beta, but only under certain poorly understood
environmental conditions. I suggest those environmental triggers have to do with
the internal manufacture of fats and cholesterol as opposed to the extraction of
these nutrients from the blood supply. I.e., amyloid-beta is produced as a
consequence of environmental oxidative stress due to an inadequate supply of
fats and cholesterol from the blood.
In addition to being utilized as an energy source by being broken down to
lactate, pyruvate can also be used as a basic building block for synthesizing
fatty acids. So anaerobic glucose metabolism, which yields pyruvate, is a
win-win-win situation: (1) it significantly reduces the risk of exposure of
fatty acids to oxygen, (2) it provides a source of fuel for neighboring neurons
in the form of lactate, and (3) it provides a basic building block for fatty
acid synthesis. But it depends upon amyloid-beta to work.
Thus, in my view (and in the view of others [28] [20]
Amyloid-Beta and Alzheimer's), amyloid-beta is not a cause
of Alzheimer's, but rather a protective device against it. The abstract of
reference [28] arguing this point of view is reproduced in full in the
Appendix.
Several variants of a genetic defect associated with amyloid precursor protein
(APP), the protein from which amyloid-beta is derived, have now been identified.
A defect in this protein, which is associated with an increased risk of early
onset Alzheimer's, would likely lead to a reduced ability to synthesize
amyloid-beta, which would then leave the brain with a big problem, since both
the fuel and the basic building blocks for fatty acid synthesis would be in
short supply, while oxygen trekking through the cell to the mitochondria would
be exposing whatever fats were being synthesized to oxidation. The cell would
likely be unable to keep up with need, and this would lead to a reduction in the
number of fatty acids in the Alzheimer's cerebrospinal fluid, a well-established
characteristic of Alzheimer's [38].
8. Cholesterol's Role in the Brain
The brain comprises only 2% of the body's total weight, yet it contains
nearly 25% of the total cholesterol in the body. It has been determined that the
limiting factor allowing the growth of synapses is the availability of
cholesterol, supplied by the astrocytes. Cholesterol plays an incredibly
important role in the synapse, by shaping the two cell membranes into a snug fit
so that the signal can easily jump across the synapse [50]. So inadequate
cholesterol in the synapse will weaken the signal at the outset, and inadequate
fat coating the myelin sheath will further weaken it and slow it down during
transport. A neuron that can't send its messages is a useless neuron, and it
only makes sense to prune it away and scavenge its contents.
The neurons that are damaged in Alzheimer's are located in specific regions
of the brain associated with memory and high level planning. These neurons need
to transmit signals long distances between the frontal and prefrontal cortex and
the hippocampus, housed in the midbrain. The transport of these signals depends
on a strong and tight connection in the synapse, where the signal is transferred
from one neuron to another, and a secure transmission across the long nerve
fiber, a part of the white matter. The myelin sheath which coats the nerve fiber
consists mainly of fatty acids, along with a substantial concentration of
cholesterol. If it is not well insulated, the signal transmission rate will slow
down and the signal strength will be severely reduced. Cholesterol is crucial
for the myelin as well as for the synapse, as demonstrated dramatically through
experiments conducted on genetically defective mice by Gesine Saher et al. [45].
These mutant mice lacked the ability to synthesize cholesterol in myelin-forming
oligodendrocytes. They had severly disturbed myelin in their brains, and
exhibited ataxia (uncoordinated muscle movements) and tremor. In the abstract,
the authors wrote unequivocally, "This shows that cholesterol is an
indispensable component of myelin membranes."
In a post-mortem study comparing Alzheimer's patients with a control group
without Alzheimer's, it was found that the Alzheimer's patients had
significantly reduced amounts of cholesterol, phospholipids (e.g, B-HDL), and
free fatty acids in the cerebrospinal fluid than did the controls [38]. This was
true irrespective of whether the Alzheimer's patients were typed as apoE-4. In
other words, reductions in these critical nutrients in the spinal fluid are
associated with Alzheimer's regardless of whether the reduction is due to
defective apoE. The reductions in fatty acids were alarming: 4.5 micromol/L in
the Alzheimer's patients, compared with 28.0 micromol/L in the control group.
This is a reduction by more than a factor of 6 in the amount of fatty acid
available to repair the myelin sheath!
People with the apoE-4 allele tend to have high serum cholesterol. The
question of whether this high cholesterol level might be an attempt on the part
of the body to adjust for a poor rate of cholesterol uptake in the brain was
addressed by a team of researchers in 1998 [39]. They studied 444 men between 70
and 89 years old at the time, for whom there existed extensive records of
cholesterol levels dating back to several decades ago. Most significantly,
cholesterol levels
fell for the men who developed Alzheimer's prior to
their showing Alzheimer's symptoms. The authors suggested that their high
cholesterol might have been a protective mechanism against Alzheimer's.
One might wonder
why their cholesterol levels fell. There was no
mention of statin drugs in the article, but statins would certainly be an
effective way to reduce cholesterol levels. The statin industry would like
people to believe that high cholesterol is a risk factor for Alzheimer's, and
they are quite thrilled that high cholesterol early in life is correlated with
Alzheimer's much later. But these results suggest quite the opposite: that blood
cholesterol levels are kept high intentionally by the body regulatory mechanisms
in an attempt to compensate for the defect. A high concentration will lead to an
increase in the rate of delivery to the brain, where it is critically needed to
keep the myelin sheath healthy and to promote neuron signaling in the synapses.
Using MRI technology, researchers at UCLA were able to measure the degree of
breakdown of myelin in specific regions of the brain [6]. They conducted their
studies on over 100 people between 55 and 75 years old, for whom they also
determined the associated apoE allele (2, 3, or 4). They found a consistent
trend in that apoE-2 had the least amount of degradation, and apoE-4 had the
most, in the frontal lobe region of the brain. All of the people in the study
were thus far healthy with respect to Alzheimer's. These results show that
premature breakdown of myelin sheath (likely due to an insufficient supply of
fats and cholesterol to repair it) is associated with apoE-4.
To summarize, I hypothesize that, for the apoE-4 Alzheimer's patients,
defective apoE has led to an impaired ability to transport fats and cholesterol
from the blood stream, via the astrocytes, into the cerebrospinal fluid. The
associated high blood serum cholesterol is an attempt to partially correct for
this defect. For the rest of the Alzheimer's patients (the ones without the
apoE-4 allele but who also have severely depleted fatty acids in their
cerebrospinal fluid), we have to look for another reason why their fatty acid
supply chain might be broken.
9. Infections and Inflammation
To summarize what I have said so far, Alzheimer's appears to be a consequence
of an inability of neurons to function properly, due to a deficiency in fats and
cholesterol. A compounding problem is that the fats over time will become rancid
if they cannot be adequately replenished. Rancid fats are vulnerable to attack
by microorganisms such as bacteria and viruses. Amyloid-beta is part of the
solution because it allows the astrocytes to be much more effective in utilizing
glucose anaerobically, which protects the internally synthesized fats and
cholesterol from toxic oxygen exposure, while at the same time providing the
energy needed both by the astrocyte for the synthesis process and by neighboring
neurons to fuel their signal firings.
Besides the astrocytes, the microglia in the brain are also implicated in
Alzheimer's. Microglia promote neuron growth when all is well, but trigger
neuron programmed cell death in the presence of toxic substances secreted by
bacteria such as polysaccharides [56]. Microglia will defensively secrete
cytokines (communication signals that promote an immune response) when exposed
to infective agents, and these in turn will lead to inflammation, another
well-known feature associated with Alzheimer's [1]. The microglia are able to
control whether neurons should live or die, and they surely base this decision
on factors related to how well the neuron functions and whether it is infected.
Once enough neurons have been programmed for cell death, the disease will
manifest itself as cognitive decline.
10. Evidence that Infection is Associated with Alzheimer's
There is substantial evidence that Alzheimer's is related to an increased
likelihood of infective agents appearing in the brain. Some researchers believe
that infective agents are the principle cause of Alzheimer's. There are a number
of bacteria that reside in the human digestive system and can co-exist with our
own cells without any harm. However, H. pylori, one that is quite common, has
been recently shown to be responsible for stomach ulcers. It has been suspected
that H. Pylori might be implicated in Alzheimer's, and, indeed, a recent study
showed that Alzheimer's patients had a significantly higher concentration of an
antibody against H. Pylori in both their cerebrospinal fluid and their blood
than non-Alzheimer's controls [26]. H. pylori was detected in 88% of the
Alzheimer's patients but only 47% of the controls. In an effort to treat the
Alzheimer's patients, the researchers administered a potent combination of
antibiotics, and assessed the degree of mental decline over the next two years
[27]. For 85% of the patients, the infection was successfully routed, and for
those patients, cognitive improvement was also detected after two years had
elapsed. So this was a nice example of the possibility of treating Alzheimer's
through antibiotics.
C. pneumoniae is a very common bacterium, estimated to infect 40-70% of
adults. But there's a big difference between a bacterium being in the blood
stream and making its way into the inner sanctum of the brain. A study of
post-mortem samples from various regions of the brains of Alzheimer's patients
and non-Alzheimer's controls revealed a remarkably different statistic: 17 out
of 19 Alzheimer's brains tested positive for the bacterium, whereas only 1 out
of 19 brains from the control group tested positive [5].
Many other infective agents, both viruses and bacteria, have been found to be
associated with Alzheimer's, including herpes simplex virus, picornavirus, Borna
disease virus, and spirochete [23]. One proposal was that a particular
bacteriophage -- a virus that infects the bacterium C. pneumoniae --
might be responsible for Alzheimer's [14]. The authors argued that the phages
might make their way into the mitochondria of the host cell and subsequently
initiate Alzheimer's.
11. Ketogenic Diet as Treatment for Alzheimer's
One of the promising new treatment paradigms for Alzheimer's is to have the
patient switch to an extremely high fat, low carb diet, a so-called "ketogenic"
diet. The name comes from the fact that the metabolism of dietary fats produces
"ketone bodies" as a by-product, which are a very useful resource for metabolism
in the brain. It is becoming increasingly clear that defective glucose
metabolism in the brain (so-called "type-3 diabetes") is an early characteristic
of Alzheimer's. Ketone bodies, whether they enter the astrocyte directly or are
produced in the astrocyte itself by breaking down fats, can be delivered to
adjacent neurons, as shown in the accompanying figure.
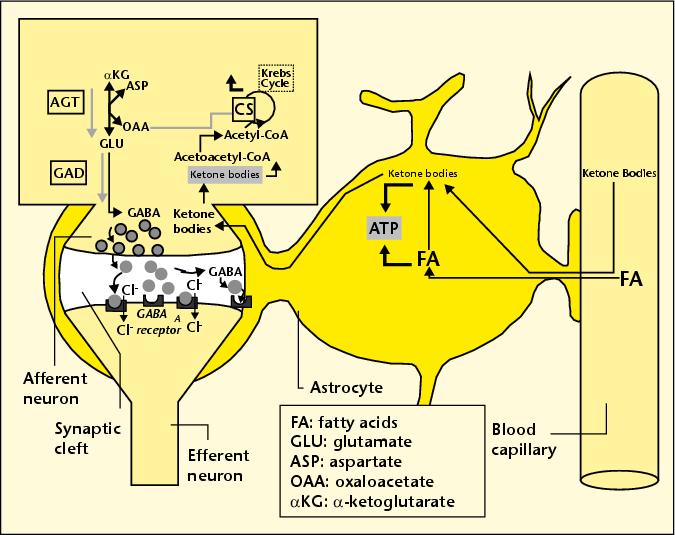
These
neurons can utilize the ketone bodies both as an energy source (replacing and
therefore relieving glucose) and as a precursor to GABA, a critical
neurotransmitter that is widespread in the brain.
Evidence that a ketogenic diet might help Alzheimer's was first found through
research conducted on mice who had been bred to be prone to Alzheimer's disease
[21]. Researchers found that the mice's cognition improved when they were
treated with a high-fat low-carb diet, and also that the amount of amyloid-beta
in their brain was reduced. The latter effect would be anticipated based on the
premise that amyloid-beta promotes full utilization of glucose anaerobically, as
I discussed previously. By having ketone bodies as an additional source of fuel,
the dependence on glucose is reduced. But another effect that may be more
important than this is the availability of high-quality fats to improve the
condition of the myelin sheath.
This idea is supported by other experiments done on human Alzheimer's
patients [11] [42]. A placebo-controlled 2004 study [42] of the effect of
dietary fat enrichment on Alzheimer's is especially informative, because it
uncovered a significant difference in effectiveness for the fat-enrichment for
subjects who did not have the apoE-4 allele as compared with those who did. The
experimental test group were given a supplemental drink containing emulsified
medium chain triglycerides, found in high concentration in coconut oil. The
subjects without the apoE-4 allele showed a significant improvement in score on
a standard test for Alzheimer's, whereas those with the apoE-4 allele did not.
This is a strong indicator that the benefit may have to do with an increase in
uptake by the astrocyte of these high-quality fats, something that the subjects
with the apoE-4 allele are unable to accomplish due to the defective IDL and LDL
transport mechanisms.
12. NADH Treatment: the Crucial Role of Antioxidants
One of the very few promising treatments for Alzheimer's is the coenzyme,
NADH (nicotinamide adenine dinucleotide) [12]. In a placebo-controlled study,
Alzheimer's subjects given NADH for six months exhibited significantly better
performances on verbal fluency, visual constructional ability and abstract
verbal reasoning than the control subjects given a placebo.
Why would NADH be effective? In the process of converting pyruvate to
lactate, lactate dehydrogenase consumes oxygen by oxidizing NADH to NAD+, as
illustrated in the accompanying figure. So, if the bioavailability of NADH is
increased, it stands to reason that the astrocyte would have an enhanced ability
to convert pyruvate to lactate, the critical step in the anaerobic metabolic
pathway that is enhanced by amyloid-beta. The process, by absorbing the toxic
oxygen, would reduce the damage to the lipids due to oxygen exposure, and would
also provide lactate as a source of energy for the neurons.
13. Excessive Oxygen Exposure and Cognitive Decline
It has been observed that some elderly people suffer temporary and sometimes
permanent cognitive decline following a lengthy operation. Researchers at the
University of South Florida and Vanderbilt University suspected that this might
be due to excessive exposure to oxygen [4]. Typically, during an operation,
people are often administered high doses of oxygen, even as much as 100% oxygen.
The researchers conducted an experiment on young adult mice, which had been
engineered to be predisposed towards Alzheimer's but had not yet suffered
cognitive decline. They did however already have amyloid-beta deposits in their
brains. The re-engineered mice, as well as a control group that did not have the
Alzheimer's susceptibility gene, were exposed to 100-percent oxygen for a period
of three hours, three times over the course of several months, simulating
repeated operations. They found that the Alzheimer's pre-disposed mice suffered
significant cognitive decline following the oxygen exposure, by contrast with
the control mice.
This is a strong indication that the excessive oxygen exposure during
operations is causing oxidative damage in the Alzheimer's brain. Given the
arguments I have presented above, this result makes good sense. The brain, by
converting to anaerobic metabolism for generating energy (with help from
amyloid-beta) is trying its best to avoid exposing the fatty acids and
cholesterol to oxidative damage. But an extremely high concentration of oxygen
in the blood makes it very difficult to protect the fats and cholesterol during
transport through the blood, and also probably causes an unavoidable increase in
oxygen uptake and therefore exposure within the brain itself.
14. Fats are a Healthy Choice!
You would practically have to be as isolated as an Australian Aborigine not
to have absorbed the message that dietary fats, particularly saturated fats, are
unhealthy. I am extremely confident that this message is false, but it is nearly
impossible to turn the opinion tide due to its pervasive presence. Most people
don't question why fats are bad; they assume that researchers must have done
their homework, and they trust the result.
To say that the current situation with regard to dietary fats is confusing
would be an understatement. We are repeatedly told to keep our total fat intake
down to, ideally, 20% of our total calories. This is difficult to achieve, and I
believe it is misguided advice. In direct contradiction to this "low-fat" goal,
we are encouraged to consume as much as possible of the "good" kinds of fats.
Fortunately, the message is finally becoming widely embraced that omega-3 fats
are healthy and that trans fats are extremely unhealthy. DHA (docosahexaenoic
acid) is an omega-3 fat that is found in large quantities in the healthy brain.
In the diet, it is available mainly from cold water fish, but eggs and dairy are
also good sources. Trans fats are generated by a high-heat process that
hydrolyzes polyunsaturated fats into a more stable configuration, which
increases their shelf life but makes them so unnatural they almost can no longer
be called a food. Trans fats are extremely damaging both to heart and brain
health. A high consumption of trans fats has recently been shown to increase the
risk of Alzheimer's [41]. Trans fats are especially prevalent in highly
processed foods -- particularly when fats are converted to a powdered form.
We are told to avoid saturated fats, mainly because they have appeared, from
empirical evidence, to be more likely to raise LDL levels than unsaturated fats.
Yet these fats are less susceptible to oxidation, and this may be why they show
up in LDL -- because they are of higher quality and therefore should
preferentially be delivered to the tissues for functional roles rather than as
fuel (i.e., free fatty acids). Coconut oil, a saturated fat, has been shown to
benefit Alzheimer's patients [42]. And high-fat dairy (also highly saturated)
has been shown to be beneficial both to fertility among women [10] and,
remarkably, to heart disease [37][22].
Despite the widespread belief that fats (particularly saturated fats) are
unhealthy, an article that appeared in the American Journal of Clinical
Nutrition in 2004 [37] claims that, for a group of post-menopausal women, a
high-fat, high-
saturated-fat diet affords better protection from coronary
artery disease than a low-fat (25% of calories from fats) diet. The subjects in
the study were obese women with coronary artery disease. Most of them had high
blood pressure, and many had diabetes. They fit the profile for
metabolic syndrome that I have previously argued is a
direct consequence of a prolonged low-fat high-carb diet. I am gratified to see
that my hypothesis that an increase in fat intake would decrease their risk of
heart disease has been verified by a carefully controlled study.
Another investigation where fats were shown to afford protection against
heart disease has just been completed. It involved a long-term study of a large
number of Swedish
men [22]. The authors looked at low- vs high-fat dairy,
as well as consumption of fruits and vegetables, meats, grains, etc. The only
statistically significant result that afforded protection from heart disease was
a combination of high-fat dairy and lots of fruits and vegetables. Fruits and
vegetables with low-fat dairy afforded no protection.
I suspect one of the critical nutrients the fruits and vegetables provide is
antioxidants that help prolong the life of the fats. Other excellent sources of
antioxidants include richly colored fruits like berries and tomatoes, coffee,
green tea, and dark chocolate, and several spices, most especially cinnamon and
turmeric (a major ingredient of curry). These should be consumed in abundance
along with fats for optimal results.
Polyunsaturated fats such as corn oil and canola oil are unhealthy for the
brain precisely because they are unsaturated. There are two major problems: (1)
they have a low melting point, which means that, if they are used for frying
they will be converted to trans fats, which are extremely unhealthy, and (2)
they are much more susceptible to becoming rancid (oxidized) at room temperature
than saturated fats, i.e., they have a shorter shelf life.
Researchers in Germany recently conducted an ingenious experiment designed to
determine how the degree of freshness of polyunsaturated fats affects the
metabolism of those fats in female lactating rats [43]. They divided female rats
into two groups, and the only difference between the test group and the controls
was that the test group was given fats that had been left in a relatively warm
place for 25 days, which caused considerable oxidative damage, whereas the
controls were fed fresh fats instead. The rats' unusual diet was begun on the
day that they gave birth to a litter. The researchers examined the mammary
glands and the milk produced by the two groups for apparent differences. They
found that the test group's milk was markedly reduced in the amount of fat it
contained, and their mammary glands correspondingly took up less fat from the
blood supply. One might surmise that the rats' metabolic mechanisms were able to
detect oxidative damage to the fats, and therefore rejected them, prefering to
do without rather than to risk the consequences of feeding their pups oxidized
fats. Consequently, the pups of the test group gained significantly less weight
than the control group's pups.
Boxed items like cookies and crackers that contain processed polyunsaturated
fats are doctored with antioxidants and even antibiotics to protect them from
spoiling. Once they're consumed, however, they still have to be protected from
going rancid. Biochemical laws work the same way whether inside or outside the
body. There are plenty of bacteria throughout the body that would be eager to
take up house-keeping in rancid fats. The body has devised all kinds of
strategies for protecting fats from oxidation (becoming rancid) and from attack
by bacteria. But its task is rendered much easier for saturated rather than
unsaturated fats, and for fresh rather than stale fats.
If we stop trying to get by on as few fats as possible in the diet, then we
don't have to become so preoccupied with getting the "right" kinds of fats. If
the body is supplied with an overabundance of fats, it can pick and choose to
find the perfect fat to match each particular need; excess or defective fats can
just be used as fuel, where it's not very important which fat it is, as long as
it can be broken down to release energy.
15. Summary and Conclusion
This is an exciting time for Alzheimer's research, as new and surprising
discoveries are coming out at a rapid pace, and evidence is mounting to support
the notion that Alzheimer's is a nutritional deficiency disease. It is an
indication of how much progress has been made in recent years to note that 42%
of the references in this essay were published in 2008 or 2009. A popular new
theory is that Alzheimer's may grow out of an impaired ability to metabolize
glucose in the brain. The term "type-3 diabetes" has been coined to describe
this defect, which often appears long before any symptoms of Alzheimer's [49]. A
shift from aerobic towards anaerobic glucose metabolism in the brain seems to be
a harbinger of Alzheimer's later in life, but I argue that the reason for this
shift is both to provide a basic ingredient (pyruvate) from which to synthesize
fatty acids, while simultaneously protecting them from potentially damaging
oxidation. The ApoE-4 allele, which is associated with increased risk to
Alzheimer's, clearly implicates defects in fat and cholesterol transport, and
the remarkable 6-fold reduction in the amount of fatty acids present in the
cerebrospinal fluid of Alzheimer's patients [38] speaks loudly the message that
fat insufficiency is a key part of the picture. The observation that the myelin
is degraded in the frontal lobes of the brains of people possessing the apoE-4
allele further substantiates the theory that the myelin repair mechanism is
defective.
Cholesterol obviously plays a vital role in brain function. A whopping 25% of
the total cholesterol in the body is found in the brain, and it is present in
abundance both in the synapses and in the myelin sheath. The cholesterol in both
of these places has been shown to play an absolutely essential role in signal
transport and in growth and repair.
Given the strong positive role played by cholesterol, it can only be assumed
that statin drugs would increase the risk of developing Alzheimer's. However,
the statin industry has been remarkably successful thus far in hiding this
painful fact. They have managed to make much of the observation that high
cholesterol much earlier in life is associated with an increased risk to
Alzheimer's thirty years later. Yet they offer not a single study, not even a
retrospective study, to substantiate any claim that actively reducing
cholesterol through statin therapy would improve the situation for these people.
In fact, most damningly, the statin usage evidence that would answer the
question was "unavailable" to the researchers who conducted the seminal study.
Beatrice Golomb is an M.D. Ph.D. who heads up the UCSD Statin Study group, a
research team who are actively investigating the risk-benefit balance of statin
drugs. She is increasingly becoming convinced that statin drugs should not be
recommended for the elderly: that in their case the risks clearly outweigh the
benefits. She makes a strong case for this position in an on-line article
available
here [15]. The section on Alzheimer's is particularly
compelling, and it points out the pitfalls in relying on previous studies done
by the statin industry, where often those who have memory problems as
side-effects of the statin drugs are excluded from the study, so that the
results end up inappropriately biased in favor of statins. In summary, she
wrote: "It must be emphasized that the randomized trial evidence has, to date,
uniformly failed to show cognitive benefits by statins and has supported no
effect or frank and significant harm to cognitive function."
In addition to refusing to take statin therapy, another way in which an
individual can improve their odds against Alzheimer's is to consume plenty of
dietary fats. It seems odd to suddenly switch from a "healthy" low-fat diet to
an extremely high fat ketogenic diet, once a diagnosis of Alzheimer's is made. A
ketogenic diet consists, ideally, of 88% fat, 10% protein, and 2% carbohydrate
[11]. That is to say, it is absurdly high in fat content. It seems much more
reasonable to aim for something like 50% fat, 30% protein, and 20% carbohydrate,
so as to pro-actively defend against Alzheimer's.
I highly recommend a recent book written by the pediatric brain surgeon,
Larry McCleary, M.D., called
The Brain Trust Program [33]. This book
gives a wealth of fascinating information about the brain, as well as specific
recommendations for ways to improve cognitive function and avert later
Alzheimer's. Most significantly, he recommends a diet that is high in
cholesterol and animal fats, including an abundance of fish, seafood, meat, and
eggs. He also recommends coconuts, almonds, avocados and cheese, all foods that
contain a significant amount of fat, while encouraging the avoidance of "empty
carbs." His knowledge on this subject grew out of his interest in helping his
young patients heal more rapidly after brain trauma.
Our nation is currently bracing itself for an onslaught of Alzheimer's, at a
time when baby boomers are approaching retirement, and our health care system is
already in a crisis of escalating costs and shrinking funds. We can not afford
the high cost of caring for the swelling population of Alzheimer's patients that
our current practices of low-fat diet and ever expanding statin usage are
promoting.
In this appendix, I include the full abstract of two papers that are
relevant to the theory presented here. The first is the abstract of reference
[19] in [46], which is reference [44] here [see the section on statin drugs
above for context]:
Abstract, "Epidemiological and clinical trials evidence about a preventive
role for statins in Alzheimer's disease:"
"This paper reviews epidemiological and clinical trials data about whether
statin use reduces the risk of Alzheimer's disease (AD). The available
information has come in three waves. The initial, mostly cross-sectional
observational reports suggested that statins might prevent dementia. Next, two
large clinical trials with cognitive add-on studies showed no benefit and
neither did the third wave, again with observational studies. The latter were
mostly longitudinal, and were critical of the first studies for not adequately
addressing confounding by indication (i.e. that patients with dementia would be
denied statins). Most recently, new data from the Canadian Study of Health and
Aging have produced a mixed result. While methodological considerations are
clearly important in understanding why the reports are so variable, there might
also be merit in differentiating between statins, based on their presumed - and
variable - mechanisms of action in dementia prevention, before concluding that
the initial reports are entirely artefactual. Still, the first reports appear to
have overestimated the extent of protection, so that unless there are important
effects achievable with specific statins, a more than a modest role for statins
in preventing AD seems unlikely." The second abstract
is taken from reference [28], on the "alternative hypothesis" that amyloid-beta
is protective rather than detrimental to Alzheimer's, i.e., that it is a
"protective response to neuronal insult:"
Abstract, "Amyloid-beta in Alzheimer disease: the null versus the
alternate hypotheses:"
"For nearly 20 years, the primary focus for researchers studying Alzheimer
disease has been centered on amyloid-beta, such that the amyloid cascade
hypothesis has become the "null hypothesis." Indeed, amyloid-beta is, by the
current definition of the disease, an obligate player in pathophysiology, is
toxic to neurons in vitro, and, perhaps most compelling, is increased by all of
the human genetic influences on the disease. Therefore, targeting amyloid-beta
is the focus of considerable basic and therapeutic interest. However, an
increasingly vocal group of investigators are arriving at an "alternate
hypothesis" stating that amyloid-beta, while certainly involved in the disease,
is not an initiating event but rather is secondary to other pathogenic events.
Furthermore and perhaps most contrary to current thinking, the alternate
hypothesis proposes that the role of amyloid-beta is not as a harbinger of death
but rather a protective response to neuronal insult. To determine which
hypothesis relates best to Alzheimer disease requires a broader view of disease
pathogenesis and is discussed herein."
References
[1] H. Akiyama, S. Barger, S. Barnum, B. Bradt, J.Bauer,
G.M. Cole, N.R. Cooper, P. Eikelenboom, M. Emmerling, B.L. Fiebich, C.E. Finch,
S. Frautschy, W.S. Griffin, H. Hampel, M. Hull, G. Landreth, L. Lue, R. Mrak,
I.R. Mackenzie, P.L. McGeer, M.K. O'Banion, J. Pachter, G. Pasinetti, C.
Plata-Salaman, J. Rogers, R.Rydel, Y. Shen, W. Streit, R. Strohmeyer, I.
Tooyoma, F.L. Van Muiswinkel, R. Veerhuis, D. Walker, S. Webster, B. Wegrzyniak,
G. Wenk, and T. Wyss-Coray, "Inflammation and Alzheimer's disease." Neurobiol
Aging (2000) May-Jun;21(3):383-421,
[2] Alzheimer's Association,
"Alzheimer's Disease Facts and Figures," Alzheimer's and Dementia (2009)
Vol. 5, Issue 3.
[3] K.J. Anstey, D.M. Lipnicki and L.F. Low, "Cholesterol
as a risk factor for dementia and cognitive decline: a systematic review of
prospective studies with meta-analysis." Am J Geriatr Psychiatry (2008)
May, Vol. 16, No. 5, pp. 343-54.
[4] G. Arendash, A. Cox, T. Mori, J.
Cracchiolo, K. Hensley, J. Roberts 2nd, "Oxygen treatment triggers cognitive
impairment in Alzheimer's transgenic mice," Neuroreport. (2009) Jun 18.
[5] B.J. Balin, C.S. Little, C.J. Hammond, D.M. Appelt, J.A. Whittum-Hudson,
H.C. Gerard, A.P. Hudson, "Chlamydophila pneumoniae and the etiology of
late-onset Alzheimer's disease." J. Alz. Dis. (2008) Vol. 13, pp.
371-380.
[6] G. Bartzokis, MD; P.H. Lu, Psy, D.H. Geschwind, MD, N.Edwards,
MA, J. Mintz, PhD, and J.L. Cummings, MD, "Apolipoprotein E Genotype and
Age-Related Myelin Breakdown in Healthy Individuals: Implications for Cognitive
Decline and Dementia," Arch Gen Psychiatry (2006) Vol. 63, pp. 63-72.
[7] N. Bernoud, L. Fenart, C. Bénistant, J. F. Pageaux, M. P. Dehouck, P.
Molière, M. Lagarde, R. Cecchelli,d, and J. Lecerf, "Astrocytes are mainly
responsible for the polyunsaturated fatty acid enrichment in blood-brain barrier
endothelial cells in vitro" Journal of Lipid Research (1998) Sept., Vol.
39, pp. 1816-1824.
[8] M. S. Brown and J. L. Goldstein, "A Receptor-Mediated
Pathway for Cholesterol Homeostasis," Nobel Lecture, December 9, 1985.
[9]
N. Cartier, C. Sevin, A. Benraiss, P. DeDeyn, D. Bonnin, M-T Vanier, M.
Philippe, V. Gieselmann and P. Aubourg, "AAV5-Mediated Delivery of Human Aryl
Sulfatase A (hARSA) Prevents Sufatide Storage and Neuropathological Phenotype in
Metachromatic Leukodystrophy (MLD) Mice," Molecular Therapy (2005) 11,
S166-S167; doi: 10.1016/j.ymthe.2005.06.431
[10] J. Chavarro, W.C. Willett,
and P.J. Skerrett, The Fertility Diet, (2008) McGraw Hill.
[11] L.C.
Costantini, L.J. Barr, J.L. Vogel and S.T. Henderson, "Hypometabolism as a
therapeutic target in Alzheimer's disease" BMC Neurosci (2008) Vol. 9,
Suppl. 2, S16. doi: 10.1186/1471-2202-9-S2-S16.
[12] V. Demarin, S.S.
Podobnik, D. Storga-Tomic and G. Kay, "Treatment of Alzheimer's disease with
stabilized oral nicotinamide adenine dinucleotide: A randomized, double-blind
study" Drugs Exp Clin Res. (2004) Vol. 30, No. 1, pp. 27-33.
[13]
R.B. DeMattos, R.P. Brendza, J.E. Heuser, M.Kierson, J.R. Cirrito, J. Fryer,
P.M. Sullivan, A.M. Fagan, X. Han and D.M. Holtzman, "Purification and
characterization of astrocyte-secreted apolipoprotein E and J-containing
lipoproteins from wild-type and human apoE transgenic mice," Neurochem
Int. (2001) Nov-Dec;39(5-6):415-25. doi:10.1016/S0197-0186(01)00049-3.
[14] M. Dezfulian, M.A. ShokrgozarA, S. Sardari, K. Parivar and G. Javadi,
"Can phages cause Alzheimer's disease?" Med Hypotheses (2008)
Nov;71(5):651-6.
[15] B.A. Golomb, M.D., Ph.D., "Statin Adverse Effects:
Implications for the Elderly," Geriatric Times (2004) May/June, Vol. V,
Issue 3
[16] W.R. Grant, Ph.D., "Does Vitamin D Reduce the Risk of
Dementia?" Journal of Alzheimer's Disease (2009) May, Vol. 17, No. 1.,
pp. 151-9.
[17] Dr. Duane Graveline, Lipitor: Thief of Memory, Statin
Drugs and the Misguided War on Cholesterol, (2004) www.buybooksontheweb.com.
[18] X. Han, "Potential mechanisms contributing to sulfatide depletion at
the earliest clinically recognizable stage of Alzheimer's disease: a tale of
shotgun lipidomics," J Neurochem (2007) November, Vol. 103, Suppl. 1. pp.
171-179. doi: 10.1111/j.1471-4159.2007.04708.x.
[19] X. Han, H. Cheng, J.D.
Fryer, A.M. Fagan and D.M. Holtzman, "Novel Role for Apolipoprotein E in the
Central Nervous System: Modulation of Sulfatide Content" Journal of
Biological Chemistry, March 7, 2003, Vol. 278, pp. 8043-8051, DOI
10.1074/jbc.M212340200.
[20] K. Heininger, "A unifying hypothesis of
Alzheimer's disease. IV. Causation and sequence of events," Rev Neurosci.
(2000) Vol. 11, Spec No, pp.213-328.
[21] S.T. Henderson, "Ketone Bodies as
a Therapeutic for Alzheimer's Disease," NeuroTherapeutics,, (2008)
Jul;5(3):470-80, doi:10.1016/j.nurt.2008.05.004
[22] S. Holmberg, A. Thelin
and E.-L. Stiernstr Nvm, "Food Choices and Coronary Heart Disease: A Population
Based Cohort Study of Rural Swedish Men with 12 Years of Follow-up," Int. J.
Environ. Res. Public Health (2009) Vol. 6, pp. 2626-2638;
[23] K. Honjo,
R. van Reekum, and N.P. Verhoeff, "Alzheimer's disease and infection: do
infectious agents contribute to progression of Alzheimer's disease?"
Alzheimers Dement. (2009) Jul;5(4):348-60.
[24] S.M. Innis and R.A.
Dyer, "Brain astrocyte synthesis of docosahexaenoic acid from n-3 fatty acids is
limited at the elongation of docosapentaenoic acid," (2002) Sept. Journal of
Lipid Research, Vol. 43, pp. 1529-1536.
[25] L. Jeng, A.V. Yamshchikov,
S.E. Judd, H.M. Blumberg, G.S. Martin, T.R. Ziegler and V. Tangpricha,
"Alterations in Vitamin D Status and Anti-microbial Peptide Levels in Patients
in the Intensive Care Unit with Sepsis," Journal of translational
Medicine," (2009) Vol. 7, No. 28.
[26] J. Kountouras, M. Boziki, E.
Gavalas, C. Zavos, G. Deretzi, N. Grigoriadis, M. Tsolaki, D. Chatzopoulos, P.
Katsinelos, D. Tzilves, A. Zabouri, I. Michailidou, "Increased cerebrospinal
fluid Helicobacter pylori antibody in Alzheimer's disease," Int J
Neurosci. (2009) 119(6):765-77.
[27] J. Kountouras, M. Boziki, E.
Gavalas, C. Zavos, N. Grigoriadis, G. Deretzi, D. Tzilves, P. Katsinelos, M.
Tsolaki, D. Chatzopoulos, and I. Venizelos, "Eradication of Helicobacter pylori
may be beneficial in the management of Alzheimer's disease," J Neurol.
(2009) May;256(5):758-67. Epub 2009 Feb 25.
[28] H.G. Lee, X. Zhu, R.J.
Castellani, A. Nunomura, G. Perry, and M.A. Smith, "Amyloid-beta in Alzheimer
disease: the null versus the alternate hypotheses," J Pharmacol Exp Ther.
(2007) June, Vol. 321 No. 3, pp. 823-9. doi:10.3390/ijerph6102626.
[29] J.
Marcus, S. Honigbaum, S. Shroff, K. Honke, J. Rosenbluth and J.L. Dupree,
"Sulfatide is essential for the maintenance of CNS myelin and axon structure,"
Glia (2006), Vol. 53, pp. 372-381.
[30] R.T. Matthews, L. Yang, S.
Browne, M. Baik and M.F. Beal, "Coenzyme Q10 administration increases brain
mitochondrial concentrations and exerts neuroprotective effects," Proc Natl
Acad Sci U S A. (1998) Jul 21, Vol. 95, No. 15, pp.8892-7.
[31] D.
Lutjohann and K. von Bergmann, "24S-hydroxycholesterol: a marker of brain
cholesterol metabolism" Pharmacopsychiatry (2003) January 10, Vol. 36
Suppl 2, pp. S102-6, DOI: 10.1055/s-2003-43053.
[32] J. C. McCann and B.N.
Ames, "Is there convincing biological or behavioral evidence linking vitamin D
deficiency to brain dysfunction?", (2008) FASEB J. Vol. 22, pp. 982-1001.
doi: 10.1096/fj.07-9326rev.
[33] Larry McCleary, M.D., The Brain Trust
Program (2007) September, The Penguin Group, New York, New York.
[34] B. McGuinness et al., "Statins for the prevention of dementia,"
Cochrane Database of Systematic Reviews, (2009) No. 2.
[35] M.M.
Mielke, P.P. Zandi, M. Sjogren, et al. "High total cholesterol levels in late
life associated with a reduced risk of dementia," Neurology (2005) Vol.
64, pp. 1689-1695.
[36] S.A. Moore, "Polyunsaturated Fatty Acid Synthesis
and Release by Brain-Derived Cells in Vitro," Journal of Molecular
Neuroscience (2001), Vol. 16, pp. 195ff.
[37] D. Mozaffarian, E.B. Rimm,
D.M. Herrington, "Dietary fats, carbohydrate, and progression of coronary
atherosclerosis in postmenopausal women," Am J Clin Nutr (2004) Vol. 80,
pp. 1175-84.
[38] M. Mulder, R. Ravid, D.F. Swaab, E.R. de Kloet, E.D.
Haasdijk, J. Julk, J.J. van der Boom and L.M. Havekes, "Reduced levels of
cholesterol, phospholipids, and fatty acids in cerebrospinal fluid of Alzheimer
disease patients are not related to apolipoprotein E4," Alzheimer Dis Assoc
Disord. (1998) Sep, Vol. 12, No. 3, pp. 198-203.
[39] I.L. Notkola, R.
Sulkava, J. Pekkanen, T. Erkinjuntti, C. Ehnholm, P. Kivinen, J. Tuomilehto, and
A. Nissinen, "Serum total cholesterol, apolipoprotein E epsilon 4 allele, and
Alzheimer's disease," Neuroepidemiology (1998) Vol. 17, No. 1, pp. 14-20.
[40] F.W. Pfrieger, "Outsourcing in the brain: Do neurons depend on
cholesterol delivery by astrocytes?", BioEssays (2003) Vol. 25 Issue 1,
pp.72-78.
[41] A. Phivilay, C. Julien, C. Tremblay, L. Berthiaume, P.
Julien, Y. Giguère and F. Calon, "High dietary consumption of trans fatty acids
decreases brain docosahexaenoic acid but does not alter amyloid-beta and tau
pathologies in the 3xTg-AD model of Alzheimer's disease." Neuroscience
(2009) Mar 3, Vol. 159, No. 1, pp. 296-307. Epub 2008 Dec 14.
[42] M.A.
Reger, S. T. Henderson, C. Hale, B. Cholerton, L.D. Baker, G.S. Watson, K. Hyde,
D. Chapman and S. Craft, "Effects of Beta-hydroxybutyrate on cognition in
memory-impaired adults," Neurobiology of Aging (2004) Vol. 25, No. 3,
March, pp. 311-314,
[43] R. Ringseis, C. Dathe, A. Muschick, C. Brandsch and
K. Eder, "Nutrient Physiology, Metabolism, and Nutrient-Nutrient Interactions
Oxidized Fat Reduces Milk Triacylglycerol Concentrations by Inhibiting Gene
Expression of Lipoprotein Lipase and Fatty Acid Transporters in the Mammary
Gland of Rats," American Society for Nutrition J. Nutr. (2007) Sept.,
Vol. 137, pp. 2056-2061.
[44] K. Rockwood, "Epidemiological and clinical
trials evidence about a preventive role for statins in Alzheimer's disease."
Acta Neurol Scand Suppl. (2006) Vol. 185, pp. 71-7.
[45] G. Saher, B.
Brugger, C. Lappe-Siefke, W. Mobius, R. Tozawa, M.C. Wehr, F. Wieland, S.
Ishibashi, and K.A. Nave, "High cholesterol level is essential for myelin
membrane growth." Nat Neurosci (2005) Apr, Vol. 8, No. 4, pp. 468-75.
Epub 2005 Mar 27.
[46] A. Solomon, M. Kivipelto, B. Wolozin, J. Zhou, and
R.A. Whitmer, "Midlife Serum Cholesterol and Increased Risk of Alzheimer's and
Vascular Dementia Three Decades Later," Dementia and Geriatric Cognitive
Disorders (2009) Vol. 28, pp. 75-80, DOI: 10:1159/000231980.
[47] M.
Simons, MD, P. Keller, PhD, J. Dichgans, MD and J.B. Schulz, MD, "Cholesterol
and Alzheimer's disease: Is there a link?" Neurology (2001) Vol. 57, pp.
1089-1093.
[48] L.L. Smith, "Another cholesterol hypothesis: cholesterol as
antioxidant," Free Radic Biol Med. (1991) Vol. 11, No. 1, pp. 47-61.
[49] E. Steen, B.M. Terry, E.J. Rivera, J.L. Cannon, T.R. Neely, R. Tavares,
X.J. Xu, J.R. Wands, and S.M. de la Monte "Impaired insulin and insulin-like
growth factor expression and signaling mechanisms in Alzheimer's disease - is
this type 3 diabetes?" Journal of Alzheiner's Disease (2005) Vol. 7,
Number 1, pp. 63-80.
[50] J. Tong, P.P. Borbat, J.H. Freed and Y-K Shin, "A
scissors mechanism for stimulation of SNARE-mediated lipid mixing by
cholesterol," PNAS (2009) March 31 Vol. 106, No. 13, pp. 5141-5146.
[51] M-C Vohl, T. A.-M. Neville, R. Kumarathasan, S. Braschi, and D.L.
Sparks, "A Novel Lecithin-Cholesterol Acyltransferase Antioxidant Activity
Prevents the Formation of Oxidized Lipids during Lipoprotein Oxidation,"
Biochemistry (1999) Vol. 38 No. 19, pp. 5976-5981. DOI:
10.1021/bi982258w.
[52] M. Waldman, MD,, 9th International Conference on
Alzheimer's and Parkinson's Diseases (2009) Abstract 90, Presented March
12-13.
[53] R. West, M.A., M. Schnaider Beeri, Ph.D., J. Schmeidler, Ph.D.,
C. M. Hannigan, B.S., G. Angelo, M.S., H.T. Grossman, M.D., C. Rosendorff, M.D.,
Ph.D., and J.M. Silverman, Ph.D., "Better memory functioning associated with
higher total and LDL cholesterol levels in very elderly subjects without the
APOE4 allele," Am J Geriatr Psychiatry (2008) September; Vol. 16, No. 9,
pp. 781-785. doi: 10.1097/JGP.0b013e3181812790.
[54] A.W.E.
Weverling-Rijnsburger, G.J. Blauw, A.M. Lagaay, D.L. Knook, A.E. Meinders, and
R.G.J. Westendorp, "Total cholesterol and risk of mortality in the oldest old,"
The Lancet, (1997) Vol. 350, No. 9085, pp. 1119-1123,
[55] R.F.
Wilson, J.F. Barletta and J.G. Tyburski, "Hypocholesterolemia in Sepsis and
Critically Ill or Injured Patients" Critical Care (2003), Vol. 7, pp.
413-414.
[56] S.-C. Zhang and S. Fedoroff, "Neuron-microglia Interactions in
Vitro," Acta Neuropathol (1996) Vol. 91, pp. 385-395.
 APOE-4: The Clue to Why Low Fat Diet
and Statins may Cause Alzheimer's
APOE-4: The Clue to Why Low Fat Diet
and Statins may Cause Alzheimer's by
Stephanie Seneff is licensed under
a
Creative
Commons Attribution 3.0 United States License.
=====================================================================
Read the complete article
here.
 In this
essay I will refer to these collectively as the XDL's. As if this weren't
confusing enough, there is also another unique XDL that is found only in the
cerebrospinal fluid, that supplies the nutritional needs of the brain and
nervous system. This one doesn't seem to have a name yet, but I will call it
"B-HDL," because it is like HDL in terms of its size, and "B" is for "brain
[13]"
In this
essay I will refer to these collectively as the XDL's. As if this weren't
confusing enough, there is also another unique XDL that is found only in the
cerebrospinal fluid, that supplies the nutritional needs of the brain and
nervous system. This one doesn't seem to have a name yet, but I will call it
"B-HDL," because it is like HDL in terms of its size, and "B" is for "brain
[13]" 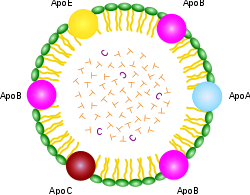 gets
what. As you can see from the schematic of the chylomicron shown at the right,
it contains a rainbow of different apo's for every conceivable application. But
the XDL's are far more specific, with HDL containing "A," LDL containing "B,"
VLDL containing "B" and "C," and IDL containing only "E." The apo's have special
binding properties that allow the lipid contents to be transported across cell
membranes so that the cell can gain access to the fats and choleseterol
contained inside.
gets
what. As you can see from the schematic of the chylomicron shown at the right,
it contains a rainbow of different apo's for every conceivable application. But
the XDL's are far more specific, with HDL containing "A," LDL containing "B,"
VLDL containing "B" and "C," and IDL containing only "E." The apo's have special
binding properties that allow the lipid contents to be transported across cell
membranes so that the cell can gain access to the fats and choleseterol
contained inside.  The internal
contents are esterified cholesterol and fatty acids, along with certain
antioxidants that are conveniently being transported to the cells packaged in
the same cargo ship. Esterification is a technique to render the fats and
cholesterol inert, which helps protect them from oxidation [51]. Having the
antioxidants (such as vitamin E and Coenzyme Q10) along for the ride is also
convenient, as they too protect against oxidation. The cholesterol contained in
the shell, however, is intentionally not esterified, which means that it is
active. One of its roles there is to guard against invasive bacteria and viruses
[55]. Cholesterol is the first line of defense against these microbes, as it
will alert the white blood cells to attack whenever it encounters dangerous
pathogens. It has also been proposed that the cholesterol in the XDL's shell
itself acts as an antioxidant [48].
The internal
contents are esterified cholesterol and fatty acids, along with certain
antioxidants that are conveniently being transported to the cells packaged in
the same cargo ship. Esterification is a technique to render the fats and
cholesterol inert, which helps protect them from oxidation [51]. Having the
antioxidants (such as vitamin E and Coenzyme Q10) along for the ride is also
convenient, as they too protect against oxidation. The cholesterol contained in
the shell, however, is intentionally not esterified, which means that it is
active. One of its roles there is to guard against invasive bacteria and viruses
[55]. Cholesterol is the first line of defense against these microbes, as it
will alert the white blood cells to attack whenever it encounters dangerous
pathogens. It has also been proposed that the cholesterol in the XDL's shell
itself acts as an antioxidant [48]. 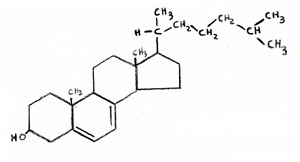 Vitamin D is synthesized from cholesterol in the skin, upon exposure to
UV rays from the sun. In fact, the chemical formula of vitamin D is almost
indistinguishable from that of cholesterol, as shown in the two attached figures
(cholesterol on the left, vitamin D on the right). If LDL levels are
Vitamin D is synthesized from cholesterol in the skin, upon exposure to
UV rays from the sun. In fact, the chemical formula of vitamin D is almost
indistinguishable from that of cholesterol, as shown in the two attached figures
(cholesterol on the left, vitamin D on the right). If LDL levels are 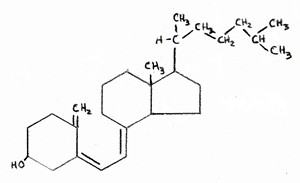 kept
artificially low, then the body will be unable to resupply adequate amounts of
cholesterol to replenish the stores in the skin once they have been depleted.
This would lead to vitamin D deficiency, which is a widespread problem in
America.
kept
artificially low, then the body will be unable to resupply adequate amounts of
cholesterol to replenish the stores in the skin once they have been depleted.
This would lead to vitamin D deficiency, which is a widespread problem in
America. 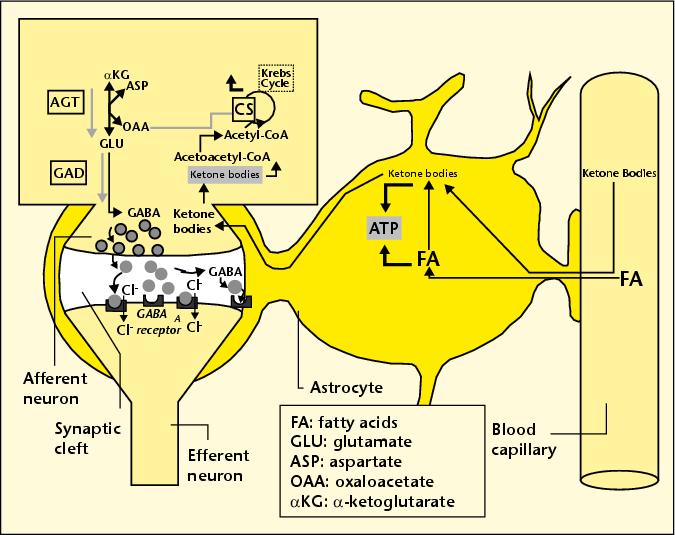 These
neurons can utilize the ketone bodies both as an energy source (replacing and
therefore relieving glucose) and as a precursor to GABA, a critical
neurotransmitter that is widespread in the brain.
These
neurons can utilize the ketone bodies both as an energy source (replacing and
therefore relieving glucose) and as a precursor to GABA, a critical
neurotransmitter that is widespread in the brain. 

No comments:
Post a Comment
I appreciate appropriate comments but reserve the right to publish those with credible, verifiable, significant information to contribute to the topic at hand. I will not post comments with commercial content nor those containing personal attacks. Thank You.